Last week, news headlines warned of a “deadly new global threat”, and social media fuelled speculation about the next pandemic.
What’s the real story? Nipah virus has reemerged in India, with two confirmed cases in West Bengal.
Nipah virus is not new. First identified during an outbreak in Malaysia in 1998-99, Nipah virus has caused sporadic outbreaks in South and Southeast Asia for more than 25 years. Its ecology and transmission pathways are well understood, and outbreaks, while sometimes severe, have historically been small and contained.
In the current outbreak, the cases are limited, closely monitored, and consistent with patterns seen repeatedly over the past two decades. Public health responses, including rapid case isolation, contact tracing, and enhanced surveillance were implemented early and decisively. Authorities have done exactly what outbreak preparedness is meant to enable: detect quickly, respond proportionately, and contain risk.
Unfortunately, the global narrative has raced ahead of the epidemiology. When an outbreak like this one occurs, reporting can frame these events as novel threats, and use emotive language and selective statistics that emphasise severity, while downplaying likelihood. Coverage can sometimes give the impression of an escalating crisis, when the actual situation is limited and contained.
In turn, this lights up the comments section with jokes about buying toilet paper, declarations of refusing future lockdowns, and warnings about mandates and lost freedoms.
These reactions are not trivial. They show how quickly outbreak coverage can activate pandemic-era fears, even when the situation does not warrant them. By collapsing different risks into the same emotional category, misinformation trains the public to react to remembered crises rather than current evidence, eroding trust and hardening resistance to public health measures before they are even relevant.
High-consequence pathogens like Nipah and Ebola viruses are particularly vulnerable to this amplification. Case fatality rates can be reported without context. The absence of a licensed vaccine is framed as a sign of vulnerability rather than as a known research gap. Spillover events are conflated with efficient human-to-human transmission.
Misinformation does not stay online. It changes behaviour. Fear-driven narratives can delay care-seeking, divert health system resources, and deepen community distrust. Outbreak panic shapes attention and fear can dominate perception, drawing focus away from measured, evidence-based responses.
This is not an argument for complacency. Nipah virus is a serious threat. It deserves sustained research investment, robust surveillance, and careful risk assessment. But seriousness does not require sensationalism. Preparedness depends on trust and trust is not easily earned, which makes reporting the facts even more critical.
So, when seeking information about an outbreak go straight to the source of truth. Here in Australia, that’s the newly formed Australian Centre for Disease Control, which brings together experts, data and evidence to give independent public health advice to government. The Centre’s advice informs government decisions about preventing and controlling diseases and preparing Australia for future health threats. What’s more, this advice is published on their website for full transparency and accountability, as embedded in the legislation.
You can find the latest advice on Nipah on the website.
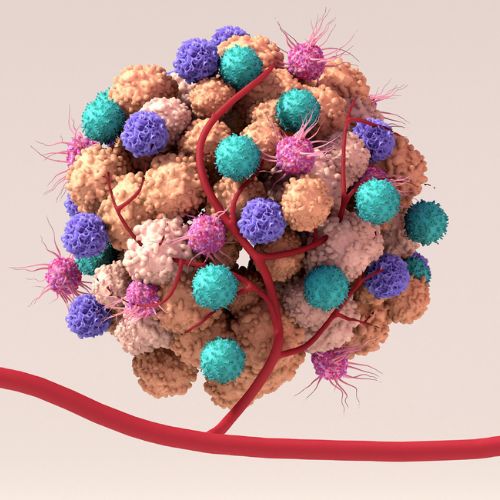
At the Victorian Infectious Diseases Reference Laboratory (VIDRL) at the Doherty Institute, we are well-prepared for Nipah virus and work closely with Victorian and Australian Government to respond to situations like these. We make sure we have the right tests in place to diagnose viruses like Nipah. We also work on finding better vaccines and treatments. All this needs to be done in a special containment facility. We have a strong collaborative relationship with institutes such as the Australian Centre for Disease Preparedness, part of the CSIRO. This ensures that cases of infectious disease are detected rapidly, managed effectively, and the public can have confidence in a measured, evidence-based response.
Fear may be contagious. But unlike viruses, it is something we can choose not to propagate.