Researchers may have developed a new way to fight drug-resistant bacteria, using specially engineered antibodies that target a sugar found only on bacterial cells. This approach allows the immune system to precisely identify harmful bacteria, potentially leading to novel treatments for hard-to-treat infections that no longer respond to antibiotics.
The sugar, called pseudaminic acid (Pse), is found exclusively on the surface of many bacterial species and plays a key role in their survival and virulence. Because Pse occurs across a wide range of bacteria, understanding it has been a long-standing challenge for researchers.
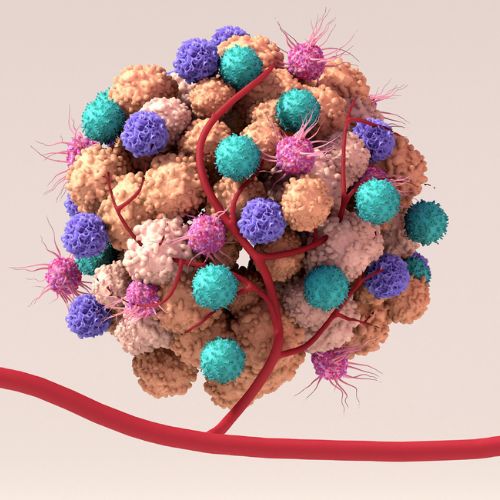
A team co-led by the University of Melbourne’s Associate Professor Nichollas Scott at the Doherty Institute, Professor Richard Payne from the University of Sydney and Professor Ethan Goddard-Borger at WEHI created antibodies that can recognise Pse with remarkable precision. By ‘flagging’ the bacteria, these antibodies help the immune system to promptly find and destroy the bacteria.

The University of Melbourne’s Kristian Karlic, PhD candidate in the Scott lab at the Doherty Institute and co-first author of the paper published in Nature Chemical Biology, said the team first chemically synthesised Pse in the lab to uncover its structure.
“We built these bacterial sugars in the lab to understand their structure, and that allowed us to create antibodies that bind to them with high precision,” said Karlic.
“Unlike most sugar-targeting antibodies, which are highly selective, the Pse antibodies we developed can bind the sugar in multiple forms and configurations. They effectively target the bacteria carrying Pse, making it easier for the immune system to find and destroy them.”
“This study shows what’s possible when we combine chemical synthesis with biochemistry, immunology, microbiology and infection biology,” said Professor Payne.
“By precisely building these bacterial sugars in the lab with synthetic chemistry, we were able to understand their shape at the molecular level and develop antibodies that bind them with high specificity. That opens the door to new ways of treating some devastating drug-resistant bacterial infections.”
The researchers test the new antibodies on well-studied drug-resistant bacteria, Helicobacter pylori, Campylobacter jejuni and Acinetobacter baumannii. In mouse infection models, the antibody successfully eliminated multidrug-resistant Acinetobacter baumannii, a major cause of hospital-acquired infections like pneumonia and bloodstream infections.
“Multidrug resistant Acinetobacter baumannii is a critical threat faced in modern healthcare facilities across the globe,” said Professor Goddard-Borger.
“It is not uncommon for infections to resist even last-line antibiotics. Our work serves as a powerful proof-of-concept experiment that opens the door to the development of new life-saving passive immunotherapies.”
Passive immunotherapy involves administering ready-made antibodies to rapidly control an infection, rather than waiting for the individual’s adaptive immune system to respond. This strategy can be used both therapeutically and prophylactically, which could be deployed to protect vulnerable patients in intensive care units.
Associate Professor Scott said the antibodies provide a powerful new tool for understanding how bacteria cause disease.
“These sugars are central to bacterial virulence, but they’ve been very hard to study,” said Associate Professor Scott.
“Having antibodies that can selectively recognise them lets us map where they appear and how they change across different pathogens.
“Our work could also pave the way for similar antibodies targeting other bacterial sugars, such as legionaminic acid and acinetaminic acid. Developing these tools could help scientists better understand bacteria and potentially lead to new therapies for drug-resistant infections.”
The team hopes to develop these antibodies into clinic-ready therapies over the next five years.
The study also benefitted from contributions from other Doherty Institute researchers: Associate Professor Maria Liaskos, who provided H. pylori strains and helped create mutant strains to validate the antibodies; Dr Glen Carter, whose team conducted the animal experiments; Associate Professor Norelle Sherry and Professor Ben Howden, who provided clinical strains to test the antibodies against multiple multidrug-resistant bacteria; and Professor Linda Wakim, who assisted with FACS experiments needed for study revisions.